22 Aug Neuropathic pain: types, causes, treatment
Pain is a subjective sensation; the occurrence, intensity, and frequency depend on numerous variables. Let’s take a closer look at a particular category: neuropathic pain.
Pain is a defense mechanism that indicates harm, real or potential. When it continues over time and becomes chronic, however, it itself becomes a disease. Chronic pain affects between 19 and 31% of the world population. Of these, it is estimated that 20% are of neuropathic origin. What is neuropathic pain?
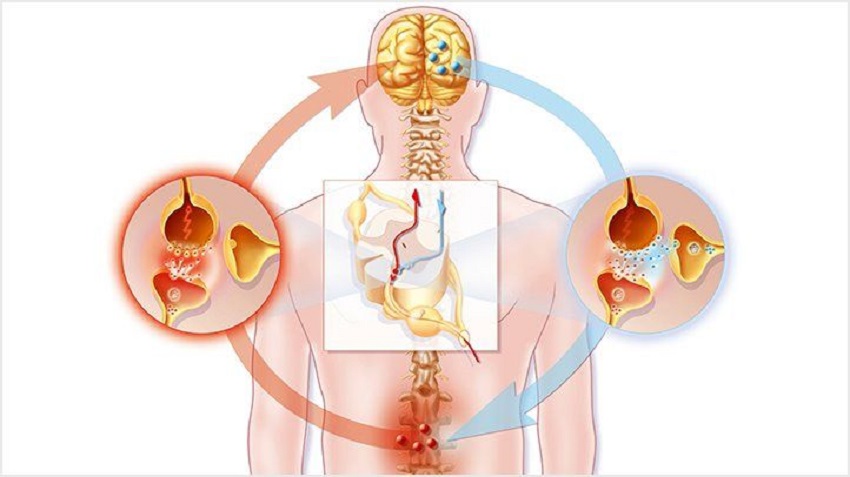
Neuropathic pain results from an injury or alteration of the central or peripheral nervous system. These provoke a painful experience even when there is no external threat, as opposed to what happens in nociceptive pain.
Nociceptive pain: unpleasant perception or sensation related to a painful stimulus; it arises, for example, when we prick ourselves with a pin.
What is neuropathic pain?
It manifests itself differently depending on the person; This ranges from mild pain to a very intense sensation. It appears following an injury to the nervous system and rarely regresses spontaneously.
Neuropathic pain: perception and sensation of pain in the absence of a painful stimulus, caused by a lesion of the nervous system.
Although we speak generically of pain, the sensations can be very different even when two people suffer from the same disease. This variability depends on causal, hereditary, and environmental factors. Neuropathic pain includes negative and positive symptoms.
The first indicators are usually negative symptoms, such as loss of sensitivity to painful stimuli or temperature. Positive symptoms resulting from a nerve injury can be spontaneous or evoked. Spontaneous symptoms include:
- Paresthesias: non-bothersome abnormalities, such as tingling.
- Dysesthesia: particularly annoying anomalies.
- Spontaneous pain: throbbing, intermittent or sharp sensation.
Evoked symptoms include:
- Allodynia: Painful perception of a non-painful stimulus, such as heat or pressure.
- Hyperalgesia: Extremely painful response to a painful stimulus.
- Hyperpathy: Delayed or explosive response to a painful stimulus.
In addition to these symptoms, people with neuropathic pain tend to develop sleep and psychological disorders.
What are the causes?
Neuropathic pain is related to an injury to the pathways that transmit painful information following a disease or injury.
The causes are so varied that four groups are usually recognized based on anatomical location or distribution:
- Asymmetric focal or multifocal lesions of the peripheral nervous system. Among these, we find post-traumatic and postoperative neuropathies, phantom limb syndrome, post-herpetic neuropathy, HIV, etc.
- Generalized lesions of the peripheral nervous system: diabetic, toxic, pharmacological, post-infectious or immunological neuropathy, etc.
- Injuries of the central nervous system: cardiovascular accidents, head injuries, multiple sclerosis, tumors, etc.
- Complex neuropathic disorders (without obvious lesions): complex regional pain syndromes of types I and II.
In non-chronic pain, the injured tissues become inflamed and cause a temporary sensitization of the area that allows the tissues to heal. However, when the pain and sensitization persist, the receptive neurons begin to behave in a maladaptive way. This causes some stimuli to cause pain or the pain to be felt more intensely.
Treatment of neuropathic pain
In order to find an effective treatment, it is necessary to start with a correct diagnosis. It is also essential to assess the presence of other pathologies that may cause pain.
Since neuropathic pain has a wide range of symptoms, an optimal combination must be found, adapted to the patient and his / her pathology.
Three drug therapies
The drugs of choice and most suitable include antidepressants, neuromodulators, and local anesthetics.
The antidepressants are tricyclic (acting on norepinephrine and are prescribed for over 25 years for neuropathic pain) or dual (act on serotonin and norepinephrine).
The neuromodulators reduce the release of glutamate, norepinephrine, and substance P . These include analgesics, anxiolytics, and antiepileptic drugs.
Topical anesthetics in the form of medicated lidocaine gel or patches are also highly recommended. When the pain is localized, they are a great, safe and effective choice.
Second-line drugs include opiates. For a long time, they have been the subject of controversy, but due to their proven effectiveness, they are prescribed in some cases, individually or in combination with other drugs.
The anticonvulsants and specific antidepressants make up the third-line group, as they have been shown to be less effective.
You may also like to read, Common Health Issues That College Freshmen Face


Sorry, the comment form is closed at this time.